Abstract
Background: Interim functional imaging (IFI) is highly prognostic in advanced classical Hodgkin Lymphoma (cHL) and can guide therapeutic decisions. Patients with positive IFI whom were escalated to BEACOPP (Johnson et al, NEJM 2016, Press et al, JCO 2016) achieved higher progression free survival (PFS) compared with historical controls who received ABVD alone. However, the benefit of IFI guided intensification remains uncertain as no direct comparison was made in recent randomized reports. Furthermore, it is unclear whether there is any overall survival (OS) advantage to this risk adapted strategy given significant improvements in salvage options over the years. This is particularly relevant as therapy related adverse events are higher with BEACOPP than ABVD including greater incidence of infertility and secondary malignancies. At our center we adopted two treatment protocols for advanced cHL; hybrid ABVD / BEACOPP or ABVD alone. The aim of this analysis is to examine the role of risk adapted therapy escalation compared to completion of ABVD.
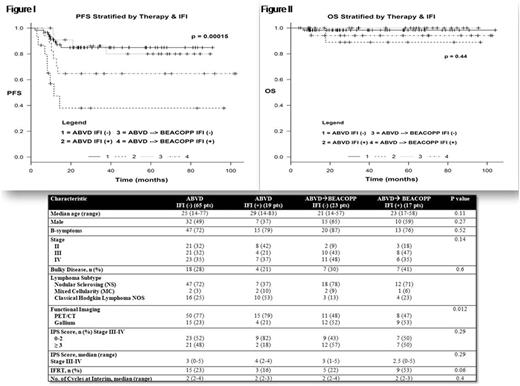
Methods: After due IRB approval, patients with cHL whom were treated at our institution from 2008 - 2016 were identified. All records were retrospectively extracted. Inclusion criteria were newly diagnosed patients with stage IIB, III or IV who received first line curative intent therapy and with IFI scan evaluation. We excluded patients with nodular lymphocyte predominant (NLP) HL, early favorable disease, patient's not receiving curative therapy and those without IFI scan. Negative PET/CT was regarded as Deauville score of ≤ 3, whereas a negative gallium was defined as no evidence of 67Ga activity. Categorical and continuous variables were compared using Pearson's chi-squared and Wilcoxon / Kruskal-Wallis, respectively. OS and PFS were computed using Kaplan-Meir method with log ranks test.
Results:
A.Baseline characteristics: We identified a total of 216 cases during this time frame, we excluded patients due to lack of IFI (52), early favorable disease (19), NLP lymphoma (13) or palliative therapy (8). A total of 124 patients were included for further analysis. Median age was 26 years (14-83) with 64 (51.6%) males. Lymphoma subtype was nodular sclerosis (67.7%), mixed cellularity (5.5%) and cHL-NOS (26.6%). Thirty four (27.4%) were stage IIB, 43 (34.7%) were stage III while 47 (37.9%) were stage IV. Bulky disease was present in 36 (29%) and 32 (25.8%) received consolidative IFRT. Eighty five (68.5%) patients underwent PET/CT while the remaining underwent gallium scan as IFI. Median number of cycles at interim was 2 (2-4). All patients were from the middle east and north Africa (MENA) region. Median follow up was 40.9 (3-132) months.
B.Risk adapted therapy stratified by IFI: Therapy administration was as follows; 84 (67.7%) received ABVD while the remaining 40 (32.3%) received ABVD followed by escalation to BEACOPP. A total of 36 (29%) patients had positive IFI and the cohort was subsequently stratified based on IFI results. Baseline features of the strata were non-significantly different as shown in table I. PFS at 2-years was significantly higher for ABVD with negative vs. positive IFI at 84.9% vs. 37.9%, respectively (p = 0.00015). Escalation to BEACOPP in cases of positive IFI also resulted in a significantly higher PFS compared to ABVD with at 64.7% vs. 37.9%, respectively. Escalation to BEACOPP compared to ABVD alone in cases of negative IFI resulted in similar PFS at 86.1% vs. 84.9% as shown in figure I. OS, was similar across the groups as shown in figure II (p=0.44). A total of 80% and 89% of relapsing patients on ABVD/BEACOPP and ABVD, respectively, received salvage followed by transplant.
Conclusion: Escalation to BEACOPP resulted in significant improvement of PFS only in cases of positive IFI. However, it remained worse than those with a negative interim scan. The lack of OS difference may be due to effective salvage therapy as most relapsing patients proceed to transplant. Although retrospective, to our knowledge this is the first direct comparison between escalation vs. completion of ABVD. Given the toxicity associated with BEACOPP, its inability to completely overcome the adverse effects of positive IFI and efficacy of salvage therapy, there is clinical equipoise to warrant prospective randomization of escalated therapy in positive IFI cases.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal